By Karen Hayes
Head injuries have a wide range of effects on an individual’s health, and one common symptom that can arise after such an injury is blurred vision which can significantly impact a person’s quality of life and ability to perform daily tasks. If you or a loved one are experiencing blurred vision after a head injury that was caused by someone else’s negligence or wrongdoing, you may be entitled to compensation. In this blog, we will discuss the importance of seeking legal representation from a skilled solicitor who specialises in head injury cases to ensure you receive the treatment and compensation you deserve.
Understanding Blurred Vision After A Head Injury
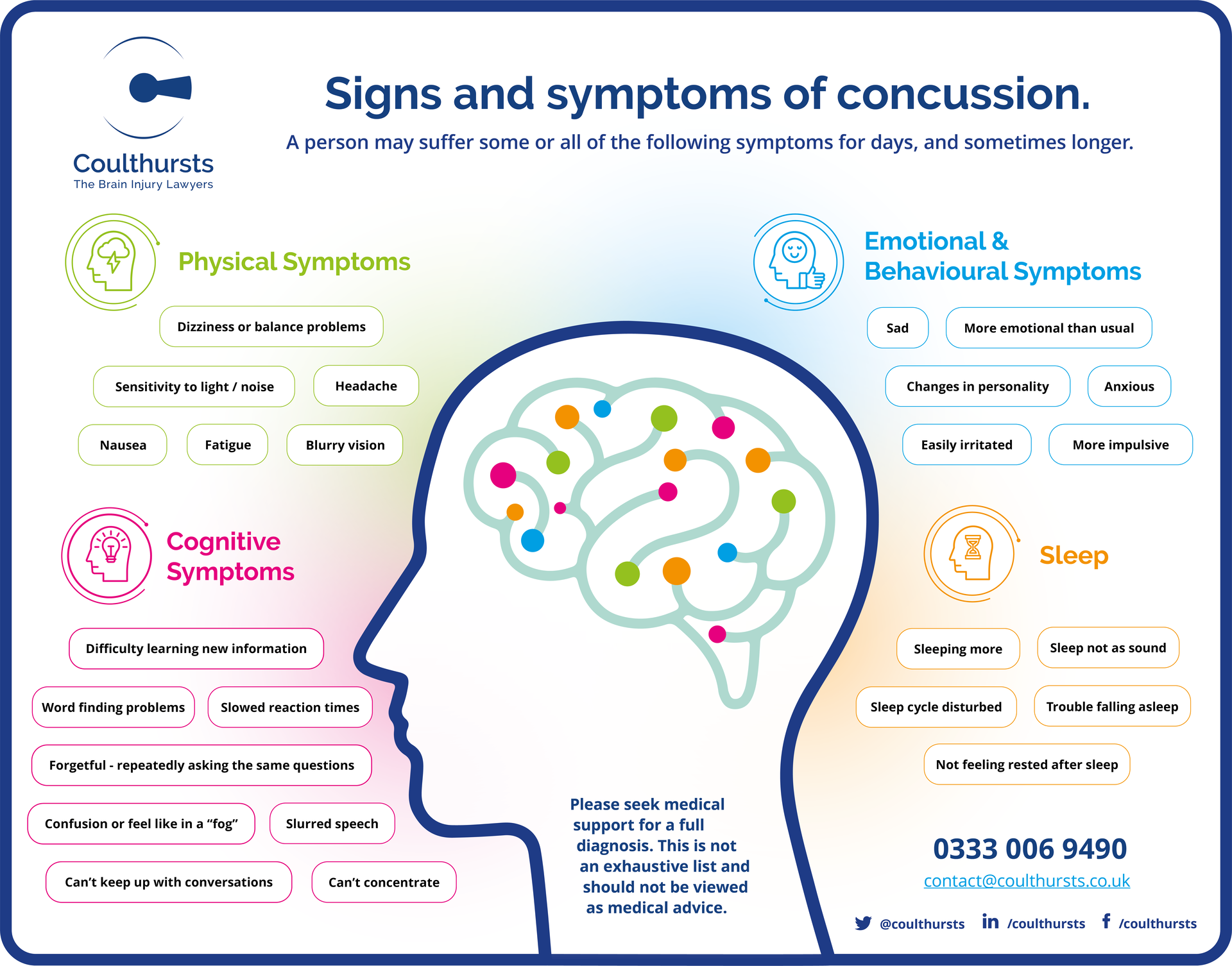
Blurred vision is a common symptom that can result from various types of head injuries, including concussions, traumatic brain injuries (TBIs) and other forms of head trauma. It occurs due to disruptions in the visual pathways to the brain or damage to the optic nerve or structures around it, resulting in an inability to focus properly. Blurred vision can range from mild blurriness to complete loss of vision in severe cases. It can be temporary or permanent, and its impact on a person’s life can be substantial.
The Role of a Head Injury Solicitor
When pursuing compensation for blurred vision after a head injury, it is crucial to have a solicitor who specialises in head injury cases by your side. Coulthursts is the only UK firm which specialises in brain injury claims and we understand the medical and legal complexities involved in such cases. Here is how we can assist you:
- Expertise
We will use our experience to assess the extent of your blurred vision and how it has impacted your life. We shall instruct an ophthalmologist to undertake a comprehensive eye examination and they will assess the changes that you have experienced after the head injury. A CT scan or MRI may also be required to identify any soft tissue or bone damage that could be the cause of the blurred vision. Once we have established the cause, we can then offer a bespoke Rehabilitation & Support Service to help you receive the best treatment possible to aid your recovery. The treatment you receive will depend on the nature and severity of the injury. All our solicitors have low caseloads, so they can spend the time necessary to support you and your loved ones at this stressful time.
- Build a strong case
We will gather your medical records, test results, and expert opinions to build a compelling case that demonstrates the connection between your head injury and your blurred vision. This may involve consultations with neurologists, ophthalmologists and other specialists.
- Calculating Compensation
Determining the appropriate amount of compensation for your case can be complex. Coulthursts Solicitors will take into account factors such as medical expenses, ongoing treatment costs, lost wages and the emotional toll of your blurred vision when calculating your claim.
- Negotiation with Insurance Companies
Insurance companies may try to settle for a lower amount than you deserve. An experienced solicitor will negotiate on your behalf to ensure you receive a fair settlement that covers all your present and future needs.
- Litigation
If a fair settlement cannot be reached through negotiation, Coulthursts will take your case to court. They will advocate for your rights and present your case effectively to a Judge to decide the value of your claim.
Conclusion
Blurred vision following a head injury can be a distressing and life-altering experience. If your injury was caused by someone else’s negligence, seeking compensation is not only your right but also essential for your recovery and well-being. To ensure the best possible outcome, it is crucial to consult with a head injury solicitor with a proven track record of handling similar cases. With our expertise, Coulthursts can help you and your loved ones navigate the legal process with confidence and we will work to ensure you receive the compensation you deserve while you focus on your recovery.
For our terms of use and disclaimer follow this link: https://coulthursts.co.uk/